Introduction
Dengue vs Typhoid – two commonly misunderstood tropical illnesses that impact millions each year, especially in developing regions. Although both diseases can lead to serious health complications if left untreated, they are caused by entirely different organisms and spread through different means. From their origins and symptoms to diagnosis and treatment strategies, understanding the clear differences between Dengue and Typhoid is essential for early detection and effective medical care. In this post, we break down the major differences between these two fevers to help you stay informed and protected.
In 2024, dengue fever reached epidemic proportions with over 14 million cases reported globally, while typhoid fever continues to affect approximately 9.3 million people worldwide each year.
According to the WHO, dengue surged in Pakistan with 48,906 cases and 183 deaths in 2021 (CFR ≈ 0.4 %), with heavy concentration in Punjab and Islamabad region. New York Post (WHO). By contrast, typhoid fever affects millions globally (9 million/year) and causes around 149,000 deaths annually (Wikipedia). Pakistan faces widespread XDR‑typhoid, with over 18,850 confirmed cases reported in Sindh alone between 2016–2020. This comprehensive guide will help you understand the key differences between these diseases, their symptoms, treatment options, and prevention strategies.
What Are Dengue and Typhoid Fever?
Dengue Fever: The Mosquito-Borne Epidemic
Dengue fever is a viral infection transmitted primarily through the bite of infected Aedes aegypti mosquitoes. The disease is caused by one of four dengue virus serotypes (DENV-1, DENV-2, DENV-3, and DENV-4). Once infected with one serotype, individuals develop lifelong immunity to that specific strain but remain susceptible to the other three. Most infections (80 %) are mild or asymptomatic; about 5 % progress to severe dengue (hemorrhage or shock) (WHO)
The disease has four clinical presentations:
- Dengue fever (DF): The mild form
- Dengue hemorrhagic fever (DHF): Severe form with bleeding
- Dengue shock syndrome (DSS): Life-threatening complication
- Severe dengue: WHO’s current classification for severe cases
Typhoid Fever: The Bacterial Infection
Typhoid fever is a bacterial infection caused by Salmonella enterica serotype Typhi (S. Typhi). Unlike dengue, typhoid spreads through contaminated food and water, making it closely linked to poor sanitation and hygiene practices. The bacteria primarily affect the intestinal tract and can spread to other organs if left untreated.
Global Disease Burden: Alarming Statistics
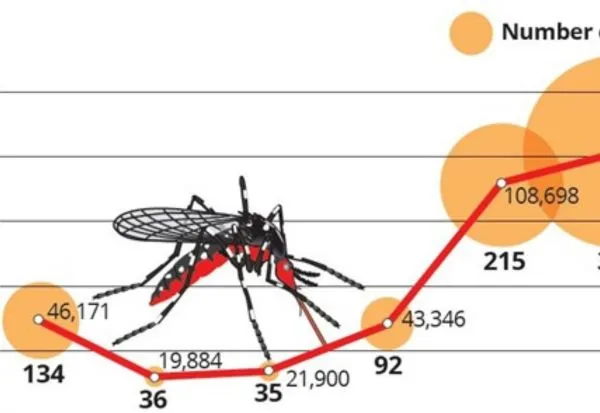
Dengue Fever Statistics 2024-2025
The dengue situation has reached critical levels:
- 2024 Global Cases: Over 14 million cases reported worldwide
- Deaths: Approximately 10,000 dengue-related deaths in 2024
- Case Fatality Rate: 0.07% globally, but varies significantly by region
- Geographic Distribution: 176 countries affected across all WHO regions
- Americas Region: Accounts for the majority of global cases (over 13 million)
- Children at Risk: In countries like Guatemala, 70% of dengue deaths occur in children
- 2025 Trend: Over 3 million cases already reported in the first quarter
Typhoid Fever Statistics 2021-2024
Typhoid remains a significant global health challenge:
- Annual Global Cases: 9.3 million cases (2021 data)
- Deaths: Approximately 107,500 deaths annually
- Case Fatality Rate: 1-4% with treatment, up to 20% without treatment
- Geographic Distribution: Highest burden in the WHO African, Eastern Mediterranean, South-East Asia, and Western Pacific Regions
- Disability-Adjusted Life Years (DALYs): 9.8 million DALYs in 2017
- US Cases: Approximately 400 culture-confirmed cases annually (2016-2018)
Key Differences: Dengue vs. Typhoid
| Feature | Dengue | Typhoid |
| Cause | Dengue virus via mosquito | Bacterial (S. Typhi) via contaminated water/food |
| Fever | Sudden high fever | Gradual + sustained high fever |
| Onset | Incubation 3–14 days, rapid progression | Slow onset over 1–2 weeks |
| Key Symptoms | Rash, headache, joint pain, bleeding | Abdominal pain, diarrhea/constipation, rash (rose spots) |
| Platelet count | Low (thrombocytopenia) | Usually normal or slight decrease |
| Treatment | Supportive (fluids, paracetamol) | Antibiotics (e.g., azithromycin, ceftriaxone) |
| CFR | 0.25–0.5 % locally | 1 % with treatment; higher in XDR cases |
| Prevention | Vector control, repellents | Clean water, hygiene, vaccination (TCV) |
Transmission Methods
Dengue Transmission:
- Primary vector: Aedes aegypti mosquitoes
- Secondary vector: Aedes albopictus
- Peak biting times: Dawn and dusk
- Breeding sites: Clean, stagnant water
- It cannot be spread person-to-person
Typhoid Transmission:
- Fecal-oral route through contaminated food/water
- Person-to-person transmission possible
- Carriers can spread infection without symptoms
- Associated with poor sanitation
- Common sources: Contaminated water, ice, food prepared by carriers
Incubation Period
- Dengue: 4-7 days (range: 3-14 days)
- Typhoid: 6-30 days (typically 8-14 days)
Symptoms and Clinical Presentation
Dengue Fever Symptoms
Early Stage (Febrile Phase – Days 1-3):
- Sudden onset of high fever (40°C/104°F)
- Severe headache
- Pain behind the eyes (retro-orbital pain)
- Muscle and joint pains
- Nausea and vomiting
- Skin rash (may appear)
Critical Phase (Days 4-6):
- Fever may subside
- Plasma leakage
- Bleeding tendencies
- Thrombocytopenia (low platelet count)
- Potential development of severe dengue
Recovery Phase (Days 7-10):
- Gradual recovery
- Fluid reabsorption
- Improvement in platelet count
Typhoid Fever Symptoms
Week 1:
- Gradual onset of fever (step-ladder pattern)
- Headache
- Malaise and weakness
- Abdominal pain
- Constipation (more common than diarrhea initially)
Week 2:
- High fever (39-40°C/102-104°F)
- Rose spots on the chest and abdomen
- Enlarged spleen
- Relative bradycardia
Week 3-4 (if untreated):
- Severe complications possible
- Intestinal bleeding
- Perforation
- Encephalitis
Laboratory Diagnosis
Dengue Diagnosis
Acute Phase (Days 1-7):
- RT-PCR for viral RNA
- NS1 antigen detection
- Viral isolation (specialized labs)
Convalescent Phase (Days 5+):
- IgM/IgG serology
- Platelet count monitoring
- Hematocrit levels
Typhoid Diagnosis
Gold Standard:
- Blood culture (most reliable)
- Bone marrow culture (highest sensitivity)
Rapid Tests:
- Widal test (limited reliability)
- Typhidot test
- Tubex test
Other Tests:
- Stool and urine cultures
- Complete blood count
Treatment Approaches
Dengue Treatment: Supportive Care
No Specific Antiviral Treatment Available
Mild Dengue:
- Adequate fluid intake
- Paracetamol for fever (avoid aspirin and NSAIDs)
- Rest and monitoring
- Oral rehydration solution
Severe Dengue:
- Hospitalization required
- Intravenous fluid therapy
- Plasma replacement
- Platelet transfusion if necessary
- Intensive monitoring
Medications to Avoid:
- Aspirin (risk of bleeding)
- NSAIDs (ibuprofen, diclofenac)
- Corticosteroids
Typhoid Treatment: Antibiotic Therapy

First-Line Antibiotics:
- Azithromycin (preferred for uncomplicated cases)
- Ceftriaxone (for severe cases)
- Ciprofloxacin (where resistance is low)
Alternative Antibiotics:
- Chloramphenicol (historically used)
- Ampicillin
- Trimethoprim-sulfamethoxazole
Treatment Duration:
- 7-14 days, depending on antibiotic choice
- Longer treatment for complicated cases
Antibiotic Resistance Concerns:
- Multidrug-resistant (MDR) strains
- Extensively drug-resistant (XDR) strains
- Fluoroquinolone resistance
Prevention Strategies
Dengue Prevention
Vector Control:
- Eliminate breeding sites (remove stagnant water)
- Use mosquito nets and repellents
- Wear long-sleeved clothing
- Community-wide larviciding programs
Vaccination:
- Dengvaxia: Available in some countries
- Recommended only for individuals with laboratory-confirmed previous dengue infection
- Not recommended for primary prevention
Environmental Management:
- Proper waste disposal
- Regular cleaning of water storage containers
- Use of biological control agents
Typhoid Prevention
Vaccination:
- Ty21a (oral live vaccine): 3-4 doses
- Vi polysaccharide (injectable): Single dose
- Effectiveness: 50-80% for 3-7 years
Water and Food Safety:
- Drink only boiled or bottled water
- Avoid ice unless made from safe water
- Eat thoroughly cooked, hot foods
- Avoid raw vegetables and fruits (unless peeled personally)
Hygiene Practices:
- Frequent handwashing with soap
- Use alcohol-based hand sanitizer
- Avoid street food in high-risk areas
- Proper sewage disposal
Complications and Prognosis
Dengue Complications
Severe Dengue Complications:
- Plasma leakage leading to shock
- Severe bleeding
- Organ involvement (liver, heart, brain)
- Death rate: 1-5% with proper medical care
Long-term Effects:
- Post-dengue fatigue syndrome
- Depression and mood changes
- Hair loss (temporary)
Typhoid Complications
Severe Complications (10-15% of cases):
- Intestinal perforation
- Gastrointestinal bleeding
- Encephalitis
- Myocarditis
- Pneumonia
Chronic Carriers:
- 2-5% become chronic carriers
- Can shed bacteria for years
- Require specific treatment protocols
Risk Factors and Vulnerable Populations
Dengue Risk Factors
Geographic Risk:
- Tropical and subtropical regions
- Urban and semi-urban areas
- Areas with poor water management
Population Risk:
- Children and the elderly
- Immunocompromised individuals
- Pregnant women
- Individuals with previous dengue infection (risk of severe disease)
Typhoid Risk Factors
Geographic Risk:
- Sub-Saharan Africa
- South and Southeast Asia
- Areas with poor sanitation
Population Risk:
- Travelers to endemic areas
- Laboratory workers
- Household contacts of cases
- Individuals with reduced stomach acid
When to Seek Medical Care
Dengue Warning Signs
Seek immediate medical attention if:
- Severe abdominal pain
- Persistent vomiting
- Bleeding
- Difficulty breathing
- Restlessness or irritability
- Sudden drop in fever with weakness
Typhoid Warning Signs
Seek immediate medical attention if:
- High fever lasting more than 3 days
- Severe abdominal pain
- Persistent headache
- Rose-colored spots on the chest
- Confusion or altered mental state
- Signs of dehydration
Global Response and Control Measures
WHO Response to Dengue
Current Initiatives:
- Global Strategy for Dengue Prevention and Control 2012-2020
- Integrated vector management programs
- Surveillance and outbreak response
- Research and development priorities
Challenges:
- Climate change is expanding mosquito habitats
- Urbanization creates breeding sites
- Limited healthcare infrastructure
- Vaccine development challenges
WHO Response to Typhoid
Current Initiatives:
- Typhoid conjugate vaccine introduction
- Water, sanitation, and hygiene (WASH) programs
- Surveillance system strengthening
- Antibiotic resistance monitoring
Progress:
- Reduced case fatality rates
- Improved vaccination coverage
- Better diagnostic methods
- Enhanced surveillance systems
Conclusion
Dengue and typhoid fever represent two distinct but equally important public health challenges affecting millions worldwide. While dengue has reached epidemic proportions in 2024 with over 14 million cases, typhoid continues to affect approximately 9.3 million people annually. Understanding the differences between these diseases is crucial for effective prevention, diagnosis, and treatment.
The key takeaways include:
- Dengue is viral and mosquito-borne, while typhoid is bacterial and spread through contaminated food/water
- Dengue treatment is supportive, while typhoid requires antibiotic therapy
- Prevention strategies differ significantly – vector control for dengue, sanitation, and vaccination for typhoid
- Both diseases can be prevented through appropriate measures and community engagement
- Early recognition and proper medical care are essential for both conditions
As global climate change and urbanization continue to expand the geographical range of these diseases, continued vigilance, improved surveillance, and strengthened healthcare systems remain our best defenses against these tropical threats.
How Al Shahbaz Hospital Helps
At Al Shahbaz Hospital, our infectious disease and tropical medicine team provides:
Rapid diagnostic testing: NS1 antigen, PCR for dengue; blood culture, Widal with antibiotic sensitivity for typhoid.Emergency management: IV fluids, platelet monitoring, and antibiotic therapy.Supportive admissions for dengue hemorrhagic fever or XDR typhoid.Preventive guidance: hygiene, vaccination, vector control awareness.
FAQs: Dengue and Typhoid Symptoms Comparison & Common Concerns
Q1: Can you get dengue and typhoid at the same time?
Yes, co-infections are possible, especially in tropical regions where both diseases are endemic. This can complicate diagnosis and treatment, requiring careful medical evaluation.
Q2: Which disease is more dangerous – dengue or typhoid?
Both can be life-threatening if untreated. Dengue has a lower overall mortality rate (0.07%) but can cause sudden, severe complications. Typhoid has a higher mortality rate (1-4% with treatment) but is more predictable in its progression.
Q3: Are there effective vaccines for both diseases?
Typhoid has effective vaccines (50-80% efficacy), while dengue vaccination is limited to specific populations with previous dengue infection. The dengue vaccine (Dengvaxia) is not recommended for primary prevention.
Q4: How long does immunity last after infection?
Dengue provides lifelong immunity to the specific serotype but not to other serotypes. Typhoid does not provide long-term immunity, and reinfection is possible.
Q5: Can pregnant women get vaccinated against these diseases?
Typhoid vaccines are generally not recommended during pregnancy unless the risk is very high. The dengue vaccine is not recommended for pregnant women.
Q6: What’s the difference between dengue and dengue hemorrhagic fever?
Dengue hemorrhagic fever is a severe form of dengue characterized by plasma leakage, bleeding, and low platelet count. It’s now classified under “severe dengue” by WHO.
Q7: Can typhoid be spread through mosquito bites?
No, typhoid is not transmitted by mosquitoes. It spreads through contaminated food and water or person-to-person contact.
Q8: Why are dengue cases increasing globally?
Factors include climate change, urbanization, increased travel, inadequate vector control, and improved surveillance leading to better reporting.
Q9: Is it safe to travel to dengue/typhoid endemic areas?
Travel is generally safe with proper precautions. For typhoid, vaccination and food/water safety measures are effective. For dengue, vector control measures are essential.
Q10: How can communities reduce the risk of these diseases?
For dengue, eliminate mosquito breeding sites, community education, and integrated vector management. For typhoid: improve sanitation, ensure a safe water supply, and promote vaccination.