Everything You Need to Know
Acid reflux is one of the major problems in the world, affecting millions of people, yet misconceptions about this common digestive condition still exist to this day. If you’ve experienced that burning sensation in your chest or wondered whether your symptoms are normal, this comprehensive guide will separate fact from fiction while providing evidence-based solutions for managing acid reflux effectively. According to the World Gastroenterology Organisation (WGO), GERD affects 20%–30% of people globally.
What is Acid Reflux? Understanding the Basics
Acid reflux occurs when stomach acid flows backward into the esophagus, the tube connecting your mouth to your stomach. This backward flow, also known as gastroesophageal reflux, happens when the lower esophageal sphincter (LES) – a ring of muscle that acts as a valve between your stomach and esophagus – doesn’t function properly.
When acid reflux becomes chronic and occurs more than twice a week, it’s classified as Gastroesophageal Reflux Disease (GERD), a more serious condition that requires medical attention. A 2023 study published in BMC Gastroenterology found that 22% of the Pakistani population reports weekly acid reflux symptoms.
The Staggering Statistics: How Common is Acid Reflux?
The prevalence of acid reflux and GERD is more widespread than many people realize:
Global Prevalence Data:
- 783.95 million people worldwide had GERD in 2019, representing a 77.53% increase from 441.57 million in 1990
- 1 in 5 people experience heartburn or acid regurgitation weekly
- 2 in 5 people experience these symptoms at least once a month
- 20% of the US population has been diagnosed with GERD, making it one of the most common digestive disorders
Regional Variations:
- North America: 18.1-27.8% prevalence
- Europe: 8.8-25.9% prevalence
- East Asia: 2.5-7.8% prevalence
- Middle East: 8.7-33.1% prevalence
- South America: 23.0% prevalence
- Australia: 11.6% prevalence
Demographics:
- Women are more likely to develop GERD than men
- Older adults show higher prevalence rates
- 10.99% overall prevalence in adults aged 35-65 years
Sources: Global Burden of Disease Study 2019, BMC Gastroenterology 2024, StatPearls NCBI
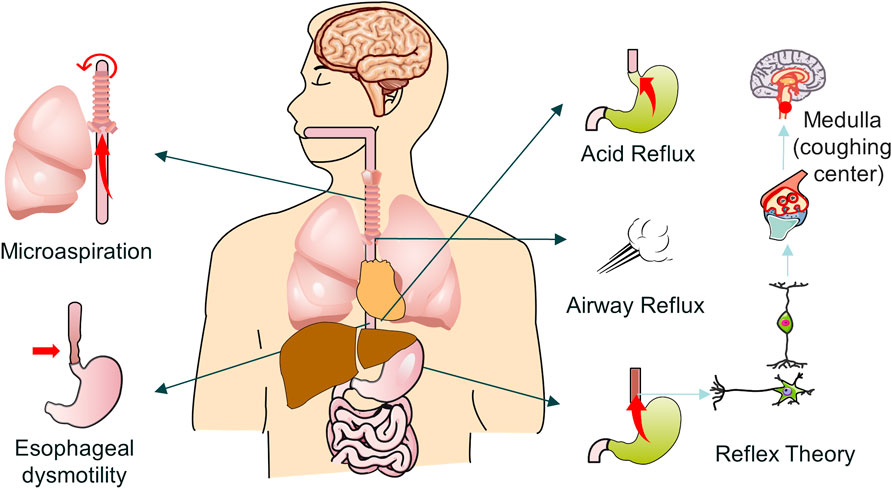
Root Causes of Acid Reflux: What Triggers It?
Understanding the true causes of acid reflux is crucial for effective management. The condition results from multiple mechanisms:
Primary Causes:
1. Lower Esophageal Sphincter (LES) Dysfunction
The LES is a complex muscular structure influenced by multiple factors:
Anatomical Factors:
- Muscle fiber orientation abnormalities
- Connective tissue disorders affecting sphincter integrity
- Aging-related muscle weakness
Physiological Factors:
- Increased transient LES relaxations (TLESRs)
- Reduced basal LES pressure
- Impaired LES response to increased abdominal pressure
Neurological Factors:
- Vagal nerve dysfunction
- Altered neurotransmitter balance (acetylcholine, nitric oxide)
- Impaired central nervous system regulation
2. Hiatal Hernia
Present in 80-90% of GERD patients, hiatal hernias disrupt normal anatomy:
Types of Hiatal Hernias:
- Type I (Sliding): 95% of cases, the stomach slides up through the diaphragm
- Type II (Paraesophageal): The Stomach herniates beside the esophagus
- Type III (Mixed): Combination of sliding and paraesophageal
- Type IV (Giant): Large portions of the stomach and other organs herniate
Impact on GERD:
- Loss of diaphragmatic support for LES
- Altered pressure dynamics
- Impaired esophageal clearance
- Increased acid exposure time
3. Delayed Gastric Emptying (Gastroparesis):
- Affects 25-50% of GERD patients
- Causes increased intragastric pressure
- Results in prolonged acid exposure
Increased Gastric Acid Production:
- Helicobacter pylori infection is paradoxically protective in some cases
- Zollinger-Ellison syndrome (rare but severe)
- Medication-induced hypersecretion
Altered Gastric Motility:
- Antral dysmotility
- Impaired antroduodenal coordination
- Abnormal migrating motor complexes
4. Increased Intra-abdominal Pressure
- Pregnancy, obesity, or tight clothing
- Forces stomach contents upward
Secondary Contributing Factors:
Lifestyle Factors:
- Smoking (reduces LES pressure)
- Alcohol consumption (relaxes LES)
- Large meals or eating late at night
- Lying down immediately after eating
Dietary Triggers:
- Spicy foods
- Citrus fruits and tomatoes
- Chocolate and caffeine
- Fatty or fried foods
- Carbonated beverages
Medical Conditions:
- Diabetes
- Asthma
- Connective tissue disorders
- Pregnancy
- Scleroderma
Medications:
- NSAIDs (ibuprofen, aspirin)
- Calcium channel blockers
- Antihistamines
- Antidepressants
Common Myths About Acid Reflux – Busted!
Myth 1: “Milk Neutralizes Stomach Acid and Soothes Heartburn”
The Dangerous Truth: While milk temporarily buffers stomach acid due to its protein content, it paradoxically stimulates increased acid production through several mechanisms:
- Protein Stimulation: Milk proteins stimulate gastrin release, increasing acid production by 30-50%
- Fat Content: Whole milk’s fat content delays gastric emptying, prolonging acid exposure
- Calcium Effect: Calcium in milk can stimulate acid production
- Rebound Acidity: Initial buffering is followed by increased acid production 1-2 hours later
Scientific Evidence: Studies show milk consumption can increase gastric acid output by up to 38% within 30 minutes. The temporary relief is often followed by worsened symptoms, creating a cycle of dependency.
Myth 2: “Apple Cider Vinegar Cures Acid Reflux.”
The Dangerous Truth: Apple cider vinegar (ACV) has a pH of 2.5-3.0, making it highly acidic and potentially harmful:
- Esophageal Damage: Can cause chemical burns to the esophagus
- Tooth Enamel Erosion: Documented cases of severe dental damage
- Delayed Gastric Emptying: May worsen gastroparesis
- Drug Interactions: Can affect medication absorption
Scientific Evidence: No peer-reviewed studies support ACV for GERD treatment. Case reports document esophageal burns, tooth damage, and worsened symptoms.
Myth 3: “Heartburn is Normal and Everyone Gets It”
The Dangerous Truth: While occasional heartburn affects most people, frequent symptoms indicate pathological GERD:
- Frequency Matters: Symptoms >2 times per week indicate GERD
- Complication Risk: Untreated GERD can lead to Barrett’s esophagus, strictures, and cancer
- Quality of Life: Chronic symptoms significantly impact daily functioning
- Progressive Disease: GERD typically worsens without treatment
Scientific Evidence: Only 5% of GERD patients develop Barrett’s esophagus, but rates of Barrett’s esophagus grew by 50% in adults ages 45-64 between 2012-2019.
Myth 4: “Antacids Are Completely Safe for Daily Use”
The Dangerous Truth: Regular antacid use can cause serious complications:
- Electrolyte Imbalances: Aluminum-based antacids can cause constipation and phosphate depletion
- Kidney Stones: Calcium-based antacids increase stone risk
- Rebound Acidity: Stopping antacids can cause increased acid production
- Nutrient Malabsorption: Chronic use affects vitamin B12, iron, and calcium absorption
- Masking Serious Conditions: May delay diagnosis of gastric cancer or other conditions
Myth 5: “Spicy Food is the Main Cause of Acid Reflux”
The Dangerous Truth: While spicy foods can trigger symptoms in some individuals, they are not a primary cause:
- Individual Variation: Only 20-30% of GERD patients report spicy food triggers
- Cultural Paradox: Populations with high spicy food consumption don’t show higher GERD rates
- Mechanism: Spicy foods may irritate already-inflamed tissues, but don’t cause initial damage
- Distraction from Real Causes: Focusing on spicy foods ignores anatomical and physiological factors
Myth 6: “Proton Pump Inhibitors Are Risk-Free”
The Dangerous Truth: Long-term PPI use carries significant risks:
- Bone Fractures: 20-30% increased risk of hip, wrist, and spine fractures
- Kidney Disease: Chronic kidney disease risk increases by 20-50%
- Infections: Increased risk of C. difficile colitis and pneumonia
- Nutrient Deficiencies: B12, magnesium, and iron deficiencies
- Dementia Risk: Some studies suggest increased dementia risk
- Dependency: Stopping PPIs can cause rebound acid hypersecretion
Myth 7: “Surgery is Always the Last Resort”
The Dangerous Truth: Modern surgical techniques can be more effective than lifelong medication.
- Laparoscopic Fundoplication: 90-95% success rate with minimal complications
- LINX Device: Magnetic sphincter augmentation with excellent outcomes
- TIF Procedure: Transoral incisionless fundoplication for select patients
- Quality of Life: Surgery often provides better symptom control than medications
Evidence-Based Treatment Options
Lifestyle Modifications (First-Line Treatment):
Dietary Changes:
- Eat smaller, more frequent meals
- Avoid trigger foods (varies by individual)
- Stop eating 2-3 hours before bedtime
- Limit alcohol and caffeine
- Maintain a food diary to identify personal triggers
Physical Modifications:
- Elevate the head of your bed 6-8 inches
- Maintain a healthy weight
- Wear loose-fitting clothes
- Avoid lying down after meals
- Quit smoking
Eating Habits:
- Chew food thoroughly
- Eat slowly
- Avoid carbonated beverages
- Limit fatty and fried foods
Medical Treatments:
Over-the-Counter Options:
- Antacids: Provide quick, temporary relief (Tums, Rolaids)
- H2 Receptor Blockers: Reduce acid production (Pepcid, Zantac)
- Proton Pump Inhibitors: Most effective for frequent symptoms (Prilosec, Prevacid)
Prescription Medications:
- Stronger PPI formulations
- Prokinetic agents (improve stomach emptying)
- Baclofen (reduces LES relaxation)
Surgical Options:
- Fundoplication (wrapping the stomach around the esophagus)
- LINX device (magnetic ring around LES)
- Transoral incisionless fundoplication (TIF)
Natural and Alternative Approaches:
Evidence-Based Natural Remedies:
- Ginger (anti-inflammatory properties)
- Chamomile tea (soothing effects)
- Licorice root (DGL form)
- Probiotics (improve gut health)
- Melatonin (promotes LES function)
Stress Management:
- Regular exercise (avoid vigorous activity after meals)
- Meditation and relaxation techniques
- Adequate sleep
- Yoga (certain poses may help)
When to See a Doctor: Red Flags
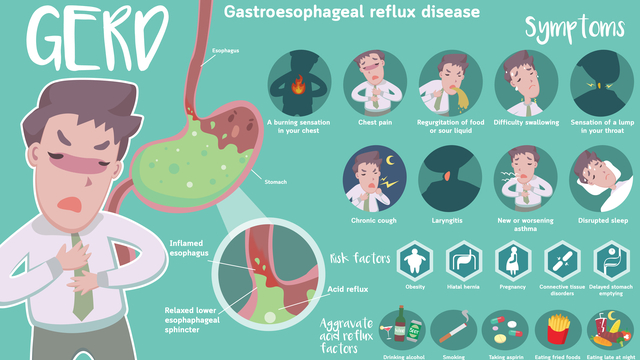
Seek immediate medical attention if you experience:
- Severe chest pain
- Difficulty swallowing
- Persistent vomiting
- Weight loss
- Blood in vomit or stool
- Symptoms that don’t improve with treatment
Schedule a doctor’s appointment if:
- Symptoms occur more than twice weekly
- Over-the-counter treatments aren’t effective
- You need antacids regularly
- Symptoms interfere with daily activities
Complications of Untreated Acid Reflux
Long-term untreated GERD can lead to serious complications:
Esophagitis: Inflammation and irritation of the esophageal lining. Strictures: Narrowing of the esophagus due to scar tissue. Barrett’s Esophagus: Precancerous changes in esophageal cells.Esophageal Cancer: Rare but serious long-term complications.n Respiratory Issues: Chronic cough, asthma exacerbation.On Dental Problems: Tooth erosion from stomach acid. A Harvard study found a 40% reduction in GERD symptoms with just a 10% weight loss.
Prevention Strategies
Dietary Prevention:
- Identify and avoid personal trigger foods
- Eat balanced, smaller meals
- Stay hydrated between meals
- Choose lean proteins and complex carbohydrates
Lifestyle Prevention:
- Maintain a healthy weight
- Regular exercise routine
- Stress management
- Proper sleep hygiene
- Avoid tight clothing
Long-term Health:
- Regular medical check-ups
- Monitor symptoms
- Medication compliance is when prescribed
- Lifestyle consistency
Why Choose Al Shahbaz Hospital?
At Al Shahbaz Hospital, our expert gastroenterologists use the latest diagnostic tools like endoscopy and pH monitoring to evaluate and treat acid reflux. Whether it’s dietary counseling, medication management, or surgical intervention, we provide personalized care.
Book your consultation now: https://alshahbazhospital.com/
Frequently Asked Questions (FAQs)
Q: How common is acid reflux?
A: Acid reflux is extremely common, affecting approximately 20% of the US population. Globally, about 784 million people had GERD in 2019, with 1 in 5 people experiencing weekly symptoms.
Q: What’s the difference between heartburn and GERD?
A: Heartburn is a symptom – the burning sensation in your chest. GERD is a chronic condition diagnosed when acid reflux occurs more than twice weekly or causes complications. You can have GERD without experiencing heartburn.
Q: Can acid reflux be cured permanently?
A: While there’s no universal “cure,” acid reflux can be effectively managed through lifestyle changes, medications, and in some cases, surgery. Many people achieve long-term symptom relief with proper treatment.
Q: Are there any foods that help with acid reflux?
A: Yes, certain foods may help: oatmeal, bananas, melons, green vegetables, lean proteins, and ginger. However, trigger foods vary by individual, so keeping a food diary is recommended.
Q: Is it safe to take antacids daily?
A: Regular antacid use should be discussed with a healthcare provider. Daily use may indicate a need for stronger treatment and could interfere with nutrient absorption or mask serious conditions.
Q: Can stress cause acid reflux?
A: Yes, stress can worsen acid reflux symptoms by increasing stomach acid production and affecting digestive function. Stress management techniques can be beneficial for symptom control.
Q: How long does it take for acid reflux treatments to work?
A: Antacids work within minutes but last 1-3 hours. H2 blockers take 30-60 minutes to work and last 4-10 hours. PPIs may take 1-4 days for full effect but provide longer-lasting relief.
Q: Can children have acid reflux?
A: Yes, acid reflux can occur in children and infants. Symptoms may include frequent spitting up, feeding problems, irritability, and respiratory issues. Consult a pediatrician if concerned.
Q: Does sleeping position affect acid reflux?
A: Yes, sleeping on your left side and elevating your head 6-8 inches can help reduce nighttime reflux by using gravity to keep stomach acid down.
Q: Are there any natural remedies that work?
A: Some evidence supports ginger, chamomile, DGL licorice, and probiotics. However, natural doesn’t always mean safe – consult healthcare providers before trying supplements.
The Bottom Line: Taking Control of Your Acid Reflux
Acid reflux is a common but manageable condition that affects millions worldwide. While myths and misconceptions persist, understanding the real causes and evidence-based treatments can help you take control of your symptoms effectively.
Remember that acid reflux isn’t just about avoiding spicy foods or drinking milk for relief. It’s a complex condition with multiple contributing factors that requires a comprehensive approach combining lifestyle modifications, appropriate medical treatment, and ongoing management.